Nerve Mechanics Part II
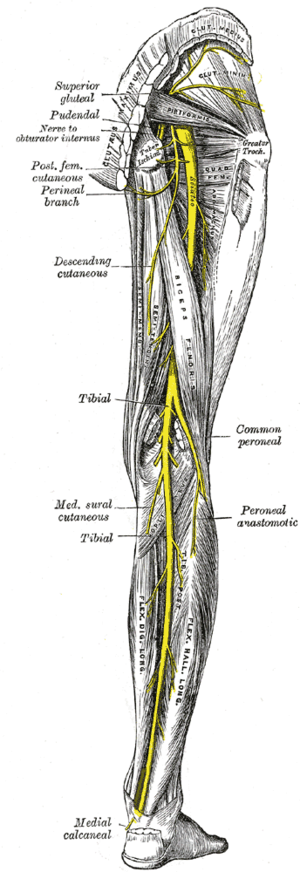
- Image via Wikipedia
In the previous post I discussed some of the basics of nerve mechanics. To review, the nerves need to slide, bend, elongate and withstand compression as the body moves. This motion is normal and helps keep the nerves healthy. Now I'll look at how nerves may become sensitive to movement and cause pain.
Healthy nerves are a top priority
First, it must be understood that maintaining healthy and functional nerves is one of the highest priorities of your central nervous system (the "CNS"). The CNS is always concerned with the health of any of its tissues and will send you an appropriate pain signal to remind you to protect them. But the nerves are uniquely important to bodily function, and therefore we should expect that any threat to the nerves is one that the CNS takes very seriously. To illustrate, if your hamstring is a little sore, you can still limp around pretty well, but if your sciatic nerve doesn't work, then you can't move or feel your leg. That's a very bad thing. So, the central nervous system will be very quick to warn you if it "thinks" that a nerve may be threatened. The warning will usually come in the form of pain, and it will arrive far in advance of the nerve actually losing function. So, what conditions in the nerves would cause the CNS to issue a pain signal?
Nerves are bloodthirsty
One potential issue is lack of blood supply. Nerves are incredibly bloodthirsty, and consume 20% of the bodies' entire oxygen supply even though they comprise only 2% of the body's weight. Nerves need a continuous supply of blood and begin to lose function rather quickly with oxygen deprivation. If a nerve is elongated 8%, the resulting tension reduces blood flow, and at 15% it ceases. This is fine in the short term, but after a while it becomes a health issue. If nerves are held at only 6% strain for one hour, nerve conduction reduces by 70%. If your nerves' blood supply is compromised by a certain posture or movement, you can be sure that your central nervous system will get you to unconsciously start fidgeting or moving around to get the blood flowing again. If this doesn't work, then the CNS will probably warn you with feelings of pins and needles, numbness or pain. If you are too drunk too heed these signals and pass out on the couch in a weird position, you may wake with a semi-useless and numb arm, which is called "Saturday night palsy."
Injury and inflammation
Another potential problem with nerves is that their connective tissue coverings may become damaged by a quick stretch or other violent movement, as might occur during sports or a fall. So that "hamstring pull" might not have been a hamstring pull - it might have been the sciatic nerve getting stretched too quick. The damage to the connective tissue covering of a nerve will be repaired with scar tissue, which might not move or slide past adjacent structures as easily as the original tissue. So even after the nerve is healed and the inflammation is gone, the roughness of the nerve in one local spot may lead to compromised mobility throughout the length of the nerve.
Another potential problem is that the nerve is being irritated by an unusually rough or protruding piece of bone, cartilege or disc. For example, all of the nerves exit the spinal cord by passing right by the bones of the vertebrae. If the bones are rough because of arthritis or simply out of position due to poor coordination or posture, this might create pressure on the nerve that the CNS finds threatening. A herniated disc may be a problem simply because it may rub on nerves (the disc itself is not innervated and feels no pain.)
All of the above conditions may cause inflammation, which makes the nerves more sensitive and also squeezes out available blood supply. Inflammation might be self perpetuating for some very complicated reasons that I won't fully get into. Part of the problem may be caused by "neurogenic inflamamation", which means that when a nerve sends a pain signal up the brain, this causes another signal to come back down to the nerve ending (an antidromic impulse) to release some chemicals that cause inflammation. The inflammation lowers the threshold for the nerve to fire, which allows more pain signals, creating a potential vicious cycle. This feedback loop likely explains a great many chronic pain conditions that are hard to get rid of, such as tennis elbow, golfers elbow, plantar fasciaitis, "carpal tunnel", a "bad rotator cuff", a "hamstring pull", low back pain, neck pain, or that nagging little pain in your traps or near your shoulder blade. Physical therapists familiar with nerve mechanics believe that a great many chronic pain conditions previously diagnosed as tendinitis, arthritis or "stiff muscles" are in fact caused by sensitive nerves.
So what does the CNS do when it concludes that a nerve is under threat? The most obvious thing to do is send a pain signal to encourage you to do something about it. Perhaps it is comforting to know that in the case of nerves, that pain signal is likely to come far in advance of the nerve actually becoming damaged or compromised in its function. Perhaps you are not comforted by this thought, but research shows that you should be, so that's why I'm telling you. David Butler and Lorimer Mosely, pain researchers extraordinaire have found that providing clients with this information, along with the general message that our "hurts do not necessarily harm us", can by itself be a therapeutic way to reduce pain.
Defense or defect?
The second and less obvious thing that the CNS will do when it feels that a nerve is under threat is to inhibit your movement in the direction that is causing the problem. This is easily done by simply tightening a muscle that moves a joint in a direction that increase nerve tension. Here is an obvious example. You can significantly decrease tension on the nerves running from the neck to the arms by raising the shoulders. Ever feel that your shoulders are too high and the traps are too tight? Maybe that's the CNS trying to reduce nerve tension to the arms. Ever feel like your hamstrings are tight? Maybe that's your CNS trying to protect the sciatic nerve, which is placed under tension when the hamstrings stretch. Why else would the muscle be tight? Muscle tension is controlled by the CNS, and muscles are tight for a reason.
This can be very important information to know, because it can prevent you from making the common mistake of trying to stretch a muscle that doesn't "want" to be stretched. If your sciatic nerve is a little inflamed, then it will not want to be placed under tension. The sciatic nerve is placed under tension by hip flexion, and also low back flexion (also foot dorsiflexion and neck flexion). In other words, a forward bend or a front kick or other "hamstring" stretch. Under these circumstances, the CNS might try to tighten the hamstrings (or maybe the low back or calves) in an effort to prevent you from flexing too far forward and hurting the sciatic. Many people will feel this tightness and make a drastic error in judgment - they conclude that the tightness is causing the pain, and that if they could get rid of the tightness the pain will go away. Of course the exact opposite is true - the pain is causing the tightness. Not knowing this, they try to stretch further. Then the CNS warns the person with some more pain. Perhaps the person then thinks, "well no pain, no gain" and then stretches further. (This is especially likely if the person is in a Bikram yoga class, the person is male, and the person on the next yoga mat is a teenage girl.) The result is that the sciatic nerve is further inflamed, the CNS is further threatened, and this creates further pain and tightness. This is of course exactly the wrong approach. In the next post I'll discuss a better one.

