Assessment of Pelvic Tilt
 How do you know where your pelvis is at? Does it rotate or tilt forward/back, left/right, up/down? A new study suggests that if your only method of finding out involves palpation of bony landmarks on the pelvis, you will likely have no clue.
How do you know where your pelvis is at? Does it rotate or tilt forward/back, left/right, up/down? A new study suggests that if your only method of finding out involves palpation of bony landmarks on the pelvis, you will likely have no clue.
In this study (full text available) the authors had the excellent idea of taking thirty five cadavers and then measuring all the bony landmarks in the pelvis to determine variations in pelvic shape between people, and between the left and right sides of the pelvis on the same person.
The information gained in the study suggests that it would be very difficult to determine the exact orientation of a client’s pelvis based solely on palpation of bony landmarks. Here’s some more detail.
Assessing anterior pelvic tilt
Many therapists believe that excessive anterior tilt of the pelvis is a significant cause of chronic pain because it increases lumbar lordosis and hip flexion. I have previously pointed out that despite the common sense appeal of this theory and its widespread acceptance, there is considerable evidence that calls it into question. Many studies have found little or no correlation between measures of anterior pelvic tilt and other similar measures (sacral angle, lumbar lordosis, thoracic kyphosis) and chronic pain. If anterior tilt was a significant cause of chronic pain, we would expect to see that people with more anterior tilt have more pain, but that is not what we consistently see.
But hey, I am open to the idea that determining the habitual position of the pelvis relative to the legs and low back might be a useful thing for a therapist to know when trying to improve a client’s movement. But the question remains, how do we do this?
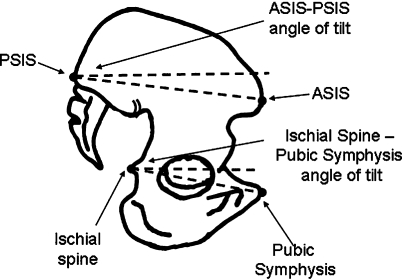 Therapists commonly assess the degree of sagittal plane pelvic tilt by comparing the height of the PSIS to the ASIS in standing. The higher the PSIS relative to the ASIS, the greater degree of anterior pelvic tilt.
Therapists commonly assess the degree of sagittal plane pelvic tilt by comparing the height of the PSIS to the ASIS in standing. The higher the PSIS relative to the ASIS, the greater degree of anterior pelvic tilt.
The problem with this method is that different people have different PSIS/ASIS angles as a result of the shape of their pelvis, not the position. In this study, even when the pelvises were in neutral*, the PSIS/ASIS angles were all over the place. The biggest difference between individuals was twenty three degrees, and the standard deviation was five degrees. This means that if you measure the standing PSIS/ASIS angle as a way to determine the degree of anterior pelvic tilt, you don't know whether you are measuring the tilt of the pelvis or the shape of the pelvis.
Assessing pelvic asymmetry
Manual therapists will often try to measure many other aspects of pelvic positioning. For example, they may assess whether the pelvis is rotated in the transverse plane or tilted in the frontal plane relative to the legs or low back. Even more complex, they may assess how one side of the pelvis is positioned relative to the other side (as a result of asymmetrical positions at the two SI joints.) Now things are getting difficult, and to succeed you better have a pretty good way of measuring pelvic position precisely. If your method relies on the implicit assumption that the right and left sides of the pelvis have the same shape (as most do), then it is likely not valid. The study shows that pelvic shape if often different from left to right.
For example, the study found that the PSIS/ASIS angle varied from left to right (up to eleven degrees), even when the pelvis was in neutral. The asymmetrical shape of the pelvis in this respect could make it appear that one side is rotated forward compared to the other.
The study also found significant differences from side to side in the height of the pelvis, as measured from the acetabulum to the iliac crest. This difference might make it appear that one leg is longer, or that the pelvis is tilted to one side in the frontal plane.
The study also found left/right differences in the angle of the iliac spine to the ASIS. I'm not sure what kind of palpation technique this difference might invalidate, but I'll take it as just more evidence in support of my guess that no matter what bony landmark you choose to measure, you can expect to find some significant differences from left to right.
This shouldn't be too surprising. We don't need sophisticated measuring techniques to look at our hands and feet and see that the bones one side are not quite like the other. We should just assume that this low grade wonkiness is pervasive.
The lesson? Make sure your assessments don't depend on an assumption that the bones are the same shape from side to side. They are probably not!
(*Note - In the study, the authors put the pelvis in “neutral” by aligning the left and right ASISes in the horizontal plane, and aligning the pubic symphysis and the ASISes in the vertical plane.)
